A SOAP note is a method of standardized note-taking used by healthcare professionals to document important information about a patient. An abbreviation for Subjective, Objective, Assessment, and Plan, millions of SOAP notes are written every single day all over the world.
Essentially, it’s the sheet of paper a physician might attach to a patient’s chart or medical file that tells other specialists everything they need to know about the patient.
However, no two SOAP notes look the same. Provider/client relationships vary across the board, from fields, workplaces, and departments.
But one thing that remains the same is the framework that every single SOAP note is built on.
Made up of four components, SOAP notes ensure that healthcare professionals can record and organize patient information clearly and cohesively. It should be easy to understand for whoever needs to interpret it.
By using this method of standardized note-taking, specialists can pass on patient files quickly and effectively. It removes the need to decipher another specialist’s observation or personal note-taking style.
Where does the SOAP note come from? A brief history

The humble SOAP note was invented in the 1950s, but it’s far cry from old fashioned. In fact, it’s widely known in the healthcare world that it paved the way for standardized medical documentation processes, thanks to Dr. Lawrence Weed.
Often referred to as the pioneer of the SOAP note, and professor of medicine and pharmacology at Yale University, Dr. Weed identified a gap in how physicians and healthcare professionals were documenting and sharing patient information. The gap was that there simply wasn’t one.
In an interview with MD Lee Jacobs at The Permanente Journal, Dr. Weed explained what had pushed him to come up with a new framework for taking notes:
The multiplicity of problems the physician must deal with every day constitutes a principal distinguishing feature between a physician’s activities and those of many other scientists.
These realizations led me to develop the POMR. So that medical students and practitioners could function in a structured, rigorous way more like that of workers in the scientific community. The POMR cannot change the multiplicity of problems that physicians face. But the POMR enables a highly organized approach to that complexity.
Dr. Weed’s new note-taking framework
To remedy what Dr. Weed believed to be a healthcare shortcoming, he began advocating for a single “scientific structure to frame clinical reasoning in the 1950s”.
In other words, Dr. Weed wanted to create notes that would help physicians identify correlations between different problems, and collaborate with one another in a seamless way.
So to enable physicians to write up notes quickly and efficiently, Dr. Weed came up with the POMR, the Problem Oriented Medical Record. This framework (which was essentially the first of its kind at that time) was considered revolutionary for healthcare by many of his peers, as was Dr. Weed himself.
In fact, in 2005, Dr. Safran at Beth Israel Deaconess Medical Center and Harvard Medical School told the New York Times: “There’s probably no one who has more fundamentally affected the way we organize our work than Larry Weed. He fundamentally changed American medicine.”
And while the POMR is still widely used by healthcare professionals, it was later developed. Fast forward a few years and it’s the very thing we’re talking about in this article. The SOAP note!
Understanding the components of a SOAP note

The SOAP note method of note-taking is made up of four components: Subjective, Objective, Assessment, and Plan. Let’s dig into each part.
Subjective
Statement about important and relevant client behavior
- In the first component, the healthcare professional enters information about the patient’s primary “complaint”, and any other problems that may be relevant
- Direct quotes from the patient
- Medical or personal issues that you think may impact the patient’s daily routine
- A complete account of the patient’s symptoms and description of ailment
- Notes and progress from any previous appointments
Here’s an example:
“Chris states: “I haven’t been eating well lately and I’ve lost my appetite”. We discussed Chris’ meal habits and work-related stresses that may be contributing to his lack of appetite. Chris states feeling pressure in his new job; during last week’s session, I recall Chris mentioning that his family expenses have increased; we talked about the possibility of this being a trigger for his stress and loss of appetite.”
Objective
Measurable, quantifiable data
- The second component of the SOAP note contains factual information about the patient’s condition, including any physical/behavioral symptoms, vital signs, physical exam results, mood observation, appearance, and diagnosis.
Here is an example: Chris is not as alert as in the last session and is responding in one-three word answers. Chris displays signs of low concentration; fiddling with his jacket buttons, looking around the room, and responding after several seconds.”
Assessment
Assimilation of Subjective and Objective sections
- The third component of the SOAP note is where the healthcare professional interprets both the subjective and objective components in order to reach a diagnosis.
- Includes relevant progress provider has seen of the client
- Includes regression or plateau of patient progress if relevant
Here is an example: “Chris appeared unusually tired during today’s session, yawning frequently and apologizing. The patient exhibited signs of anxiety and concern over his current financial situation. The patient appears to exhibit signs of disordered eating
Provider feels that the increase in financial responsibilities in his household is causing the client anxiety and this may contribute to the low appetite and unhealthy food choices.
Plan
Details the course of action for the treatment plan to help other physicians understand what the next steps are
- The final component outlines the recommended course of action
- Includes any additional testing or visits to address the patient’s issue
- Includes any specialist referrals or consultations
Here is an example: “Patient will consult with a licensed nutritionist to evaluate current eating habits and create a healthy diet plan. Eating disorder therapy has been recommended to the patient.”
Why are SOAP notes so beneficial to healthcare providers?

So we’ve covered the components of the SOAP note. Let’s look at why it’s so beneficial for health practitioners to implement it in their daily workflows.
When it comes to teamwork and decision-making, the healthcare industry is one that can’t afford to cut corners. One of the most pressing reasons why healthcare practitioners swear by this standardized method of note-taking is that it drastically reduces the risk of miscommunication between specialists.
Think about it. If each provider records patient notes however they want, in whichever order and fashion they see fit, sharing and passing information along would be inefficient and extremely challenging. Not to mention it would be an open gateway to both human and business error, which we know can lead to malpractice.
Choosing the SOAP note route, however, allows easy legibility for anyone who needs to interpret a patient’s medical file.
It’s vital that providers can carry out their care without the nagging worry that they’ve misinterpreted the previous provider’s notes; not only does it reduce stress but it empowers the provider to do what they do best without second-guessing themselves.
By writing SOAP notes, specialists can spend less time trying to decipher medical notes, and more time delivering care to their patients.
Here are even more reasons why SOAP notes are invaluable to healthcare providers:
- It’s faster
Healthcare providers are taking notes all day, so it’s hardly a surprise that a systemized note-taking method has the power to drastically reduce admin time.
There’s no need to gather external notes or come back to a patient’s file the next day because you missed a crucial piece of information. SOAP notes have a specific, clear structure and it stays the same regardless of who the patient may be. All you need to do is follow it.
- Encourages a more intelligible framework
As with all processes, the longer you use it, the more natural it becomes to do so.
This is great for healthcare, in particular, as specialists can take what they know from the SOAP note method and apply it to other areas of their day, such as meetings with colleagues or patient appointments.
The SOAP note method is highly practical and logical, so it provides a great foundation for approaching patient interactions.
- Allows easier communication between specialists
Usually, more than one specialist will have access to a patient’s medical record, which means multiple people will be reading and interpreting the same sheet of paper.
SOAP notes help healthcare providers work together by offering a clear, simple, and easy-to-read format that tells specialists everything they need to know. Messy, illegible patient notes, be gone!
What do SOAP notes look like?
So far, we’ve covered what the SOAP note actually is, how it came about, the distinct components that structure it, and why it’s so beneficial for healthcare providers. It’s time to look at a SOAP note in the flesh.
Example of a SOAP NOTE
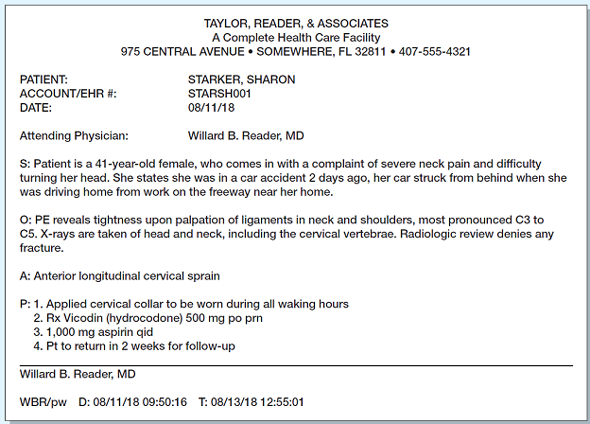
In this example, taken from the student learning platform Chegg, we can clearly see the four components of the SOAP note.
Starting with the S component (Subjective), the provider states subjective information about the patient – age, complaint, and a brief statement reporting what the patient has shared.
O component (Objective): the provider notes certain statistics about the patient – height, weight, etc, as well as factual information and observations about her physical state, previous scan, and diagnosis.
A component (Assessment): the provider shares an informed assessment based on Subjective and Objective notes, in this case, a cervical sprain.
Finally, the P section (Plan) clearly states the provider’s recommended course of action.
Now, if we were to look at any other SOAP note, all the above information would be different, especially if the patient has attended multiple visits.
But as we mentioned earlier on in this article, the one thing that remains identical in all SOAP notes is that they are written using the exact same framework, regardless of who is writing them, and who they’re being written about.
The standardization, brevity, and succinctness are all characteristics that define the SOAP note, and thanks to this simplicity, healthcare providers can read and interpret them quickly and with clarity.
Write your own flawless SOAP notes
Writing one type of SOAP note is easy enough, but if you need to take notes for several different types of SOAP notes, eg. medical, surgical, etc, then you’ll want an easier, time-efficient way to do so – and Fat Finger can help!
Here’s how
With Fat Finger, you can essentially create any type of checklist or procedure that you need in a matter of seconds, and then automate that workflow and turn it into a template.
So whenever you and your team need to write a SOAP note, you can instantly grab the right template and get writing.
What’s more, Fat Finger’s smart drag and drop nature makes it ridiculously easy to create various SOAP note templates so you can finally ditch the pen and paper route and digitize each step of your paper-based processes. That’s less time on admin time and more time to deliver care and collaborate with your team.
Here’s how Fat Finger can drastically improve and simplify your SOAP note process using intelligent automation:
- Speed up the SOAP note process – templates decrease the time spent note-taking by cutting out paper-based processes. No more faffing trying to find paper documents or referring back to past notes!
- Enhance quality control – by automating and standardizing the SOAP note process, you automatically improve its quality by removing ambiguity and ensuring everything you write is eligible and easy to interpret.
- Security and flexibility – you can’t retrieve past SOAP notes as quickly as when they’re automated. If you work within multiple facilities, the freedom to quickly pull up reports and other documentation as and when you need them can save you not just masses of time but a whole lot of burnout too.
- Track SOAP notes over time – SOAP notes are a great way to standardize medical note-taking but it doesn’t provide a way to track your documentation over time. When you automate your notes with Fat Finger, you can create reports and track metrics to help you better understand patient needs.
Create flawless SOAP notes faster with Fat Finger
SOAP notes are an essential tool to help healthcare providers deliver the best care possible without losing time remembering, documenting, and sharing patient information.
In a profession where efficiency and time management are paramount, the humble SOAP note makes it possible for providers to collaborate seamlessly.
Ready to start writing your own flawless SOAP notes? Sign up to Fat Finger and learn more about ditching those bulky, time-consuming paper processes so you can finally automate your SOAP notes. It’s faster, easier, and guaranteed to save you a ton of time and headache.